

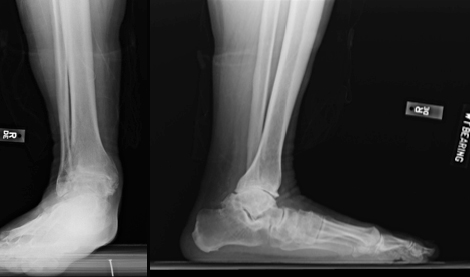
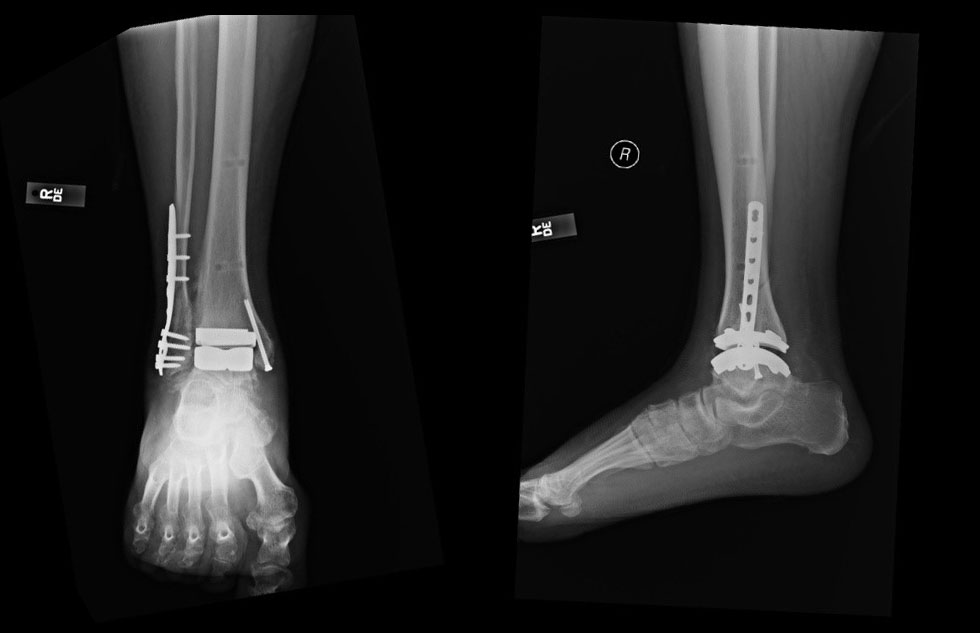
Total ankle arthroplasty is an alternative to arthrodesis for end-stage osteoarthritis in select patients with significant pain.1 While ankle fusion has traditionally been the standard of care for these patients, the advancement of surgical techniques, instrumentation, and implants has allowed total ankle replacement to become a reliable and reproducible treatment option – providing equivalent pain relief without sacrificing the motion of the ankle joint. Long-term outcomes of total ankle arthroplasty demonstrate good-to-excellent results with significant pain relief, good functional outcomes, and high patient satisfaction.2-4
“Over the last 10 years, the advancements in total ankle arthroplasty have been tremendous. Improvements in the instrumentation as well as the implants have allowed for ankle replacements to be a reproducible, pain-relieving, and motion preserving procedure. With long-term outcomes comparable to those seen with ankle fusions, ankle replacements are challenging our previous perception that fusion is the gold standard treatment for end-stage ankle arthritis,” said Eric W. Tan, MD, assistant professor of clinical orthopaedic surgery at Keck School of Medicine of USC.
Although total ankle arthroplasty is increasing in popularity, a ‘high-volume’ foot and ankle surgeon may only perform 15 to 20 ankle replacements per year. Therefore, experience matters. Current practice guidelines recommend that total ankle replacement be performed by “foot and ankle orthopaedic surgeons with special training and adequate experience in arthroplasty techniques.”1
Devices available for total ankle arthroplasty include those that are introduced by an anterior approach, and a recently developed device that is introduced by a lateral transfibular approach.5 The lateral approach may provide a benefit over the anterior approach in terms of direct visualization of the center of joint rotation, to allow for accurate alignment and reduce the bony resection needed to place the prosthesis.5
“While there are many different approaches and implants that can be used, one of the most important factors when considering an ankle replacement is who is performing your surgery, in particular the experience they have. There is a significant learning curve associated with ankle replacements, so patients want to find a surgeon who has the appropriate training and experience, as this will be important to achieving a good outcome,” said Tan.
Overcoming Challenges
The most challenging aspect of all joint replacements, especially total ankle arthroplasty, is restoring or maintaining the proper alignment of the prosthesis components. Appropriate preoperative planning with consideration of bone cuts and soft tissue balancing remains essential to ensure that the implants are placed anatomically. Even small deviations from anatomic alignment will result in poor performance and decreased longevity of the implant. The small size of the ankle joint makes this a meticulous, but important, task.
Surgeons at Keck Medicine of USC understand how to approach patients with complex total ankle arthroplasty cases. We are highly experienced in ankle arthroplasty and comfortable taking on challenging cases, whether it’s a patient with a significant deformity of the ankle, or someone who needs a revision procedure.
Patient Selection
Patients who are typical candidates for total ankle arthroplasty include those over the age of 50 or 60 years who do not routinely perform high-impact activities, and those who can adhere to postoperative rehabilitation and prophylaxis.
Careful patient selection is critical; not every patient with a degenerative ankle joint is a good candidate for total ankle arthroplasty. For example, a patient with arthritis secondary to a fracture of the talar neck may have avascular necrosis (dead bone) in the ankle joint. Ankle arthroplasty in this type of patient has a high risk of failure.6 In these cases, ankle arthrodesis is the best option to reduce pain and prevent further damage.
The Keck Effect
Patients undergoing ankle arthroplasty can benefit from the multidisciplinary care at Keck Medicine of USC, including readily available consultation with plastic surgeons or vascular surgeons; management of comorbidities by specialists across the organization; and stabilization and optimization of the patient’s condition before surgery. In addition, Keck has an extensive network of physiotherapists who are attuned to the specific needs of patients following ankle arthroplasty.
References
- American Orthopaedic Foot and Ankle Society. Total ankle replacement (TAR). https://www.aofas.org/PRC/conditions/Documents/Total-ankle-replacement.pdf. Accessed July 5, 2018.
- Chou LB, Coughlin MT, Hansen S, Jr, Lundeen G, Saltzman CL, Mann RA. Osteoarthritis of the ankle: The role of arthroplasty. J Am Acad Orthop Surg. 2008;16(5):249-259.
- Jastifer JR, Coughlin MJ. Long-term follow-up of mobile bearing total ankle arthroplasty in the united states. Foot Ankle Int. 2014;36(2):143-150.
- Gougoulias N, Khanna A, Maffulli N. How successful are current ankle replacements? A systematic review of the literature. Clin Orthop Relat Res. 2010;468:199-208.
- Tan EW, Maccario C, Talusan Pg, Schon LC. Early complications and secondary procedures in transfibular total ankle replacement. Foot Ankle Int. 2016;37(8):835-841.
- Calvert E, Younger A, Penner M. Post talus neck fracture reconstruction. Foot Ankle Clin N Am. 2007;12:137-151.
